Waking up with jaw pain, facial tightness, or persistent headaches is not something most people immediately associate with a dental condition. Yet for millions of individuals, these symptoms are the daily consequences of teeth grinding, clinically known as bruxism. Often silent and unnoticed, bruxism can gradually damage teeth, overload jaw joints, and significantly affect quality of life.
At Frederick Prime Dental, we regularly see patients who have tried mouth guards, stress reduction, and lifestyle changes with only partial relief. For some, muscle-driven clenching remains severe. In these cases, Botox® for teeth grinding has emerged as a clinically effective, non-surgical treatment option.
This in-depth guide explores bruxism from diagnosis to advanced treatment, with a particular focus on Botox therapy—how it works, who it is for, benefits, limitations, and what patients should realistically expect.
Understanding Teeth Grinding (Bruxism)
Bruxism is the involuntary clenching or grinding of the teeth. It can occur during sleep (sleep bruxism) or while awake (awake bruxism). Many patients are unaware they grind their teeth, especially when it happens at night, until symptoms or dental damage become evident.
Common Signs and Symptoms of Bruxism
Bruxism affects more than just the teeth. Symptoms may include:
-
Jaw pain or stiffness, especially in the morning
-
Facial muscle soreness or fatigue
-
Frequent tension-type headaches or migraines
-
Tooth sensitivity without obvious decay
-
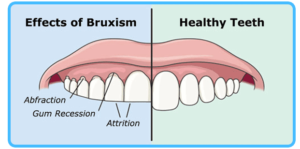
Flattened, chipped, or cracked teeth
-
Clicking or pain in the temporomandibular joint (TMJ)
-
Ear pain or a sensation of fullness without infection
-
Poor sleep quality or partner disturbance due to grinding sounds
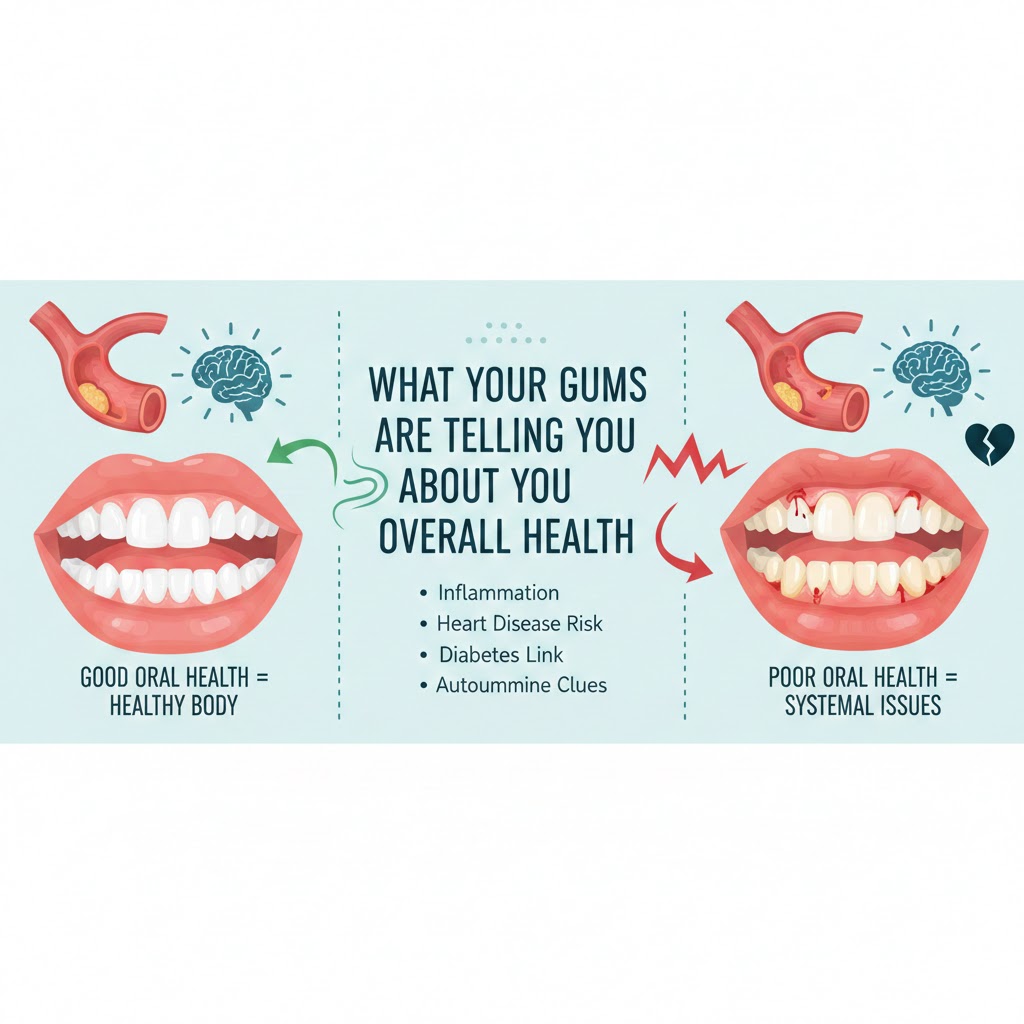
Over time, untreated bruxism can lead to advanced tooth wear, fractures, gum recession, and chronic TMJ disorders.

Why Do People Grind Their Teeth?
Bruxism is multifactorial, meaning it rarely has a single cause. Common contributing factors include:
1. Stress and Anxiety
Emotional stress remains one of the most common triggers. Clenching is often an unconscious physical response to mental tension.
2. Sleep Disorders
Conditions such as sleep apnea increase the likelihood of nighttime grinding.
3. Bite and Occlusal Issues
Misaligned teeth or an uneven bite may contribute to abnormal muscle activity.
4. Neuromuscular Factors
Overactivity of the jaw muscles, particularly the masseter and temporalis muscles, plays a central role.
5. Lifestyle Factors
Caffeine, alcohol, smoking, and certain medications can increase muscle activity during sleep.
Understanding the underlying contributors is essential when determining the most appropriate treatment approach.
Traditional Treatments for Bruxism
Before considering Botox, most patients will try conventional therapies, including:
Night Guards and Occlusal Splints
Custom dental guards protect teeth from wear but do not stop muscle activity. Grinding often continues beneath the appliance.
Stress Management
Relaxation techniques, exercise, and therapy may help when stress is a dominant factor.
Physical Therapy and Jaw Exercises
These can improve muscle balance and joint mobility but may not fully control clenching.
Bite Adjustments
In select cases, correcting occlusion may reduce symptoms.
For patients with persistent muscle-driven bruxism, these methods may provide protection but not adequate symptom relief. This is where Botox becomes a valuable option.
What Is Botox and Why Is It Used for Bruxism?
Botox® (botulinum toxin type A) is a purified neurotoxin that temporarily reduces muscle contraction by blocking nerve signals. While widely known for cosmetic use, Botox has decades of medical applications, including treatment for migraines, muscle spasticity, and jaw disorders.
In bruxism, Botox is used to relax overactive jaw muscles, primarily the masseter muscles, and sometimes the temporalis muscles.
How Botox Works for Teeth Grinding
The masseter muscles are responsible for forceful jaw closure and chewing. In patients with bruxism, these muscles are often hypertrophic (overdeveloped) and excessively active.
The Mechanism
-
Botox is injected directly into the targeted jaw muscles
-
It reduces the intensity and frequency of muscle contractions
-
Clenching force decreases, even if some grinding motion remains
Importantly, Botox does not paralyze the muscles. Normal chewing, speaking, and facial expressions are preserved when treatment is performed correctly.
The Botox for Bruxism Treatment Process
1. Comprehensive Consultation
A detailed evaluation is essential. This includes:
-
Medical and dental history
-
Assessment of jaw muscle size and tenderness
-
Evaluation of tooth wear and TMJ function
-
Discussion of symptoms and previous treatments
Botox is not a one-size-fits-all solution. Dosage and injection sites must be tailored to each patient.
2. The Injection Procedure
-
The skin is cleaned and prepared
-
Small amounts of Botox are injected into specific points of the masseter (and sometimes temporalis) muscles
-
The procedure typically takes 10–15 minutes
-
Anesthetic is usually unnecessary
Most patients describe the sensation as a mild pinch.
3. Aftercare
-
Normal activities can usually be resumed immediately
-
Avoid heavy jaw exercise or massage for 24 hours
-
Mild tenderness or swelling may occur temporarily
When Will You See Results?
Botox does not work instantly. Typical timelines include:
-
3–5 days: Early reduction in muscle tension
-
7–14 days: Full therapeutic effect
-
3–6 months: Duration of symptom relief
As the Botox gradually wears off, muscle activity slowly returns. Repeat treatments are commonly scheduled to maintain results.
Benefits of Botox for Teeth Grinding
1. Effective Pain Relief
By reducing excessive muscle force, Botox alleviates jaw pain, facial soreness, and tension headaches.
2. Protection of Teeth and Restorations
Lower clenching forces reduce the risk of tooth wear, fractures, and damage to crowns or veneers.
3. Improved Sleep Quality
Less grinding often leads to more restful sleep for both patients and their partners.
4. Reduced TMJ Strain
Botox can decrease stress on the jaw joints, helping manage TMJ-related symptoms.
5. Facial Aesthetic Benefits
In some patients, gradual reduction in masseter size leads to a softer, slimmer jawline—an additional benefit for those with muscle hypertrophy.
Potential Risks and Side Effects
Botox is considered safe when administered by experienced clinicians. However, patients should be informed of possible side effects:
Common and Mild
-
Temporary swelling or bruising
-
Mild jaw fatigue
-
Headache shortly after treatment
Less Common
-
Temporary weakness when chewing very hard foods
-
Slight asymmetry in facial movement
Rare
-
Difficulty chewing or speaking clearly
-
Spread of toxin to nearby muscles
-
Allergic reactions
Proper technique, conservative dosing, and clinical expertise significantly reduce these risks.
Who Is a Good Candidate for Botox for Bruxism?
Botox may be appropriate if you:
-
Experience chronic jaw pain or headaches linked to clenching
-
Have visible tooth wear despite wearing a night guard
-
Have enlarged or tender jaw muscles
-
Have not achieved sufficient relief with conventional treatments
Botox may not be suitable for patients who are pregnant, breastfeeding, or have certain neuromuscular conditions.
Botox vs Night Guards: Do You Need Both?
Botox and night guards serve different purposes:
-
Night guards protect teeth from damage
-
Botox reduces muscle force and pain
In many cases, using both together provides optimal protection and symptom control.
How Often Do You Need Botox for Bruxism?
Most patients require treatment every 3 to 6 months. Over time, repeated treatments may lead to longer-lasting relief as muscle strength gradually decreases.
Treatment frequency is always individualized based on response and symptom recurrence.
Long-Term Considerations
Botox does not cure the underlying causes of bruxism, such as stress or sleep disorders. For long-term management, a comprehensive approach may include:
-
Stress management strategies
-
Sleep evaluations
-
Dental monitoring
-
Ongoing muscle therapy
Botox should be viewed as part of a multidisciplinary treatment plan, not a standalone cure.

Final Thoughts
Bruxism is more than a bad habit—it is a complex neuromuscular condition that can significantly impact dental health and overall well-being. For patients with persistent symptoms driven by excessive jaw muscle activity, Botox offers a scientifically supported, non-surgical solution.
By targeting the source of clenching rather than just protecting the teeth, Botox can provide meaningful relief, improved comfort, and long-term dental preservation when delivered by experienced professionals.
Frequently Asked Questions
Does Botox completely stop teeth grinding?
Botox reduces muscle force and frequency but may not eliminate all grinding movements.
Is Botox for bruxism painful?
Most patients report minimal discomfort during injections.
Can Botox affect my smile or facial expressions?
When performed correctly, facial movement remains natural.
How soon can I eat after treatment?
You can eat normally right away, though very hard foods may feel uncomfortable temporarily.
Is Botox for teeth grinding safe long-term?
Studies support its safety when administered at appropriate doses by trained clinicians.